Osteoporosis is a skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to an increased risk of fractures. The condition often progresses silently, with no noticeable symptoms until a fracture occurs.
Bone is a dynamic tissue constantly undergoing remodeling, and in osteoporosis, the balance between bone formation and resorption is disrupted, resulting in weakened bones.
Arthritis on the other hand, refers to inflammation of the joints and encompasses a diverse group of conditions. Arthritis is of 2 major types; osteoarthritis and rheumatoid arthritis.
Risk Factors of Osteoporosis
- Age and Gender: Osteoporosis is more common in postmenopausal women due to hormonal changes. However, it can affect men and women of all ages.
- Hormonal Changes: Reduced estrogen levels in postmenopausal women and low testosterone levels in men can contribute to bone loss.
- Family History: Genetics plays a role, and individuals with a family history of osteoporosis may be at a higher risk.
- Nutrition and Lifestyle: Inadequate calcium and vitamin D intake, sedentary lifestyle, smoking, and excessive alcohol consumption increase the risk.
Clinical manifestations of osteoporosis: Osteoporosis primarily manifests through fractures, especially in the hip, spine, and wrist. These fractures can have severe consequences on an individual’s mobility and quality of life. Another manifestation is loss of height, as compression fractures in the spine can result in a stooped posture.
Diagnosis and Management of Osteoporosis
- Bone Density Testing: Dual-energy X-ray absorptiometry (DEXA) scans are commonly used to measure bone mineral density and assess fracture risk.
- Medications: Bisphosphonates, hormone replacement therapy, and other medications may be prescribed to prevent bone loss and reduce fracture risk.
- Lifestyle Interventions: Adequate calcium and vitamin D intake, weight-bearing exercises, and lifestyle modifications are crucial for managing osteoporosis.
Types of Arthritis
The two most prevalent types are Osteoarthritis and Rheumatoid arthritis. However there are other less common types of arthritis too.
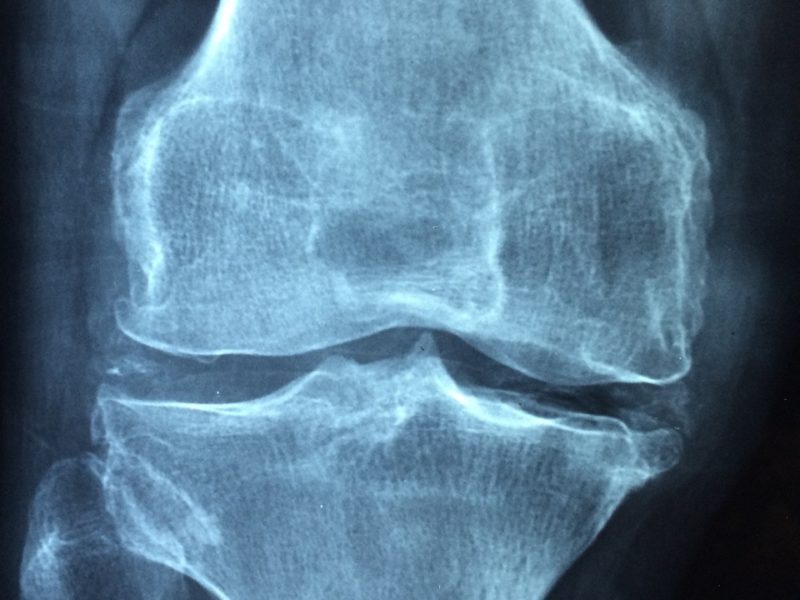
- Osteoarthritis (OA): this is the most common form of arthritis, characterized by the gradual wearing down of joint cartilage. It typically affects weight-bearing joints like the knees, hips, and spine. It is caused by aging, joint injury, obesity, and genetic factors contribute to the development of OA.
Symptoms include joint pain, stiffness, tenderness, reduced flexibility, and, in advanced stages, bone spurs.
- Rheumatoid Arthritis (RA): this is an autoimmune disorder where the immune system attacks the synovium, causing inflammation and joint damage. The exact cause of this condition is unknown, but it involves a combination of genetic and environmental factors.
Symptoms include joint pain, swelling, morning stiffness, fatigue, and potentially deformities in the affected joints.
Other types of Arthritis
- Psoriatic Arthritis (PsA) occurs in some individuals with psoriasis, an autoimmune skin condition that affects the joints and may involve the skin, nails, and eyes. Genetic predisposition and immune system dysfunction contribute to PsA. It can be characterized by joint pain, stiffness, swollen fingers and toes, nail changes, and skin patches.
- Ankylosing Spondylitis (AS) primarily affects the spine, causing inflammation and potentially leading to fusion of the vertebrae. It is most common in males and has a strong genetic component.
- Gout is caused by the accumulation of uric acid crystals in joints, leading to inflammation and intense pain. Symptoms may include sudden and severe joint pain, swelling, redness, and tenderness, commonly in the big toe.
- Lupus Arthritis or Systemic lupus erythematosus (SLE) is an autoimmune disease that can involve multiple organs, including the joints. Complex autoimmune factors triggered by genetic and environmental elements may cause this and symptoms may include joint pain, swelling, and stiffness, along with other systemic manifestations like skin rashes and fatigue.
- Juvenile Idiopathic Arthritis (JIA) refers to arthritis that occurs in individuals under the age of 16, and it encompasses several subtypes. The exact causes are not well understood and it can greatly impact a child’s growth and development.
- Reactive Arthritis is a form of arthritis that develops in response to an infection, often in the urinary or gastrointestinal tract. This infection triggers an abnormal immune response, leading to joint inflammation.
- Septic Arthritis results from a bacterial infection in a joint, leading to inflammation.
Diagnosis and Management of Arthritis
- Clinical Evaluation: A detailed medical history, physical examination, and imaging studies help diagnose arthritis and determine its type.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and corticosteroids are commonly prescribed.
- Physical Therapy: Exercises to improve joint function, strengthen muscles, and maintain flexibility are integral to arthritis management.
- Surgery: In severe cases, joint replacement surgery may be considered to alleviate pain and improve joint function.
Common Ground between Osteoporosis and Arthritis
While osteoporosis and arthritis are distinct conditions, they share certain connections:
- Bone Health: Both conditions impact bone health. Osteoarthritis affects the cartilage within joints, and rheumatoid arthritis may lead to bone erosion.
- Mobility Challenges: Pain and stiffness in joints can restrict mobility in both osteoporosis and arthritis, affecting daily activities.
- Quality of Life: The chronic nature of these conditions can significantly impact an individual’s quality of life, necessitating comprehensive management strategies.
Overlapping Strategies
Exercise Benefits: Weight-bearing exercises beneficial for osteoporosis can also help arthritis patients by promoting joint flexibility and muscle strength.
Nutrition: Adequate calcium and vitamin D intake is crucial for both conditions, though dietary needs may vary.
Holistic Approach: Combining pharmacological interventions with lifestyle changes creates a holistic approach to managing both osteoporosis and arthritis.